
The healthcare sector has entered a defining decade of digital transformation. From electronic health records (EHRs) to AI-enabled diagnostic systems, healthcare organizations have invested billions in technology meant to improve outcomes, enhance operational efficiency, and empower clinicians. Yet, many institutions still fail to realize the full value of their digital investments. The issue is rarely the technology itself. It lies in how effectively people use it.
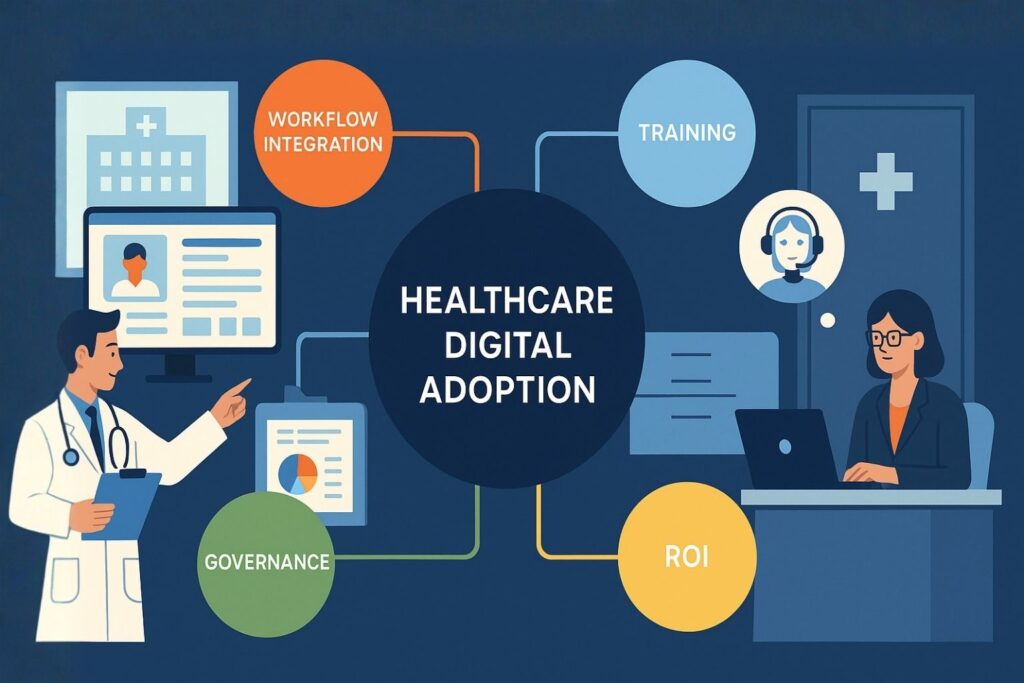
Healthcare Digital Adoption has become the critical factor separating successful transformation initiatives from those that underperform. True adoption is more than rolling out new platforms or offering initial training. It represents the sustained integration of technology into everyday clinical, operational, and administrative behavior. When adoption succeeds, it transforms not only workflows but also the entire organizational culture that drives healthcare delivery.
In this article, we will explore why digital adoption is the linchpin of healthcare success, the unique barriers hospitals face, and the frameworks required to embed adoption as a strategic competency.
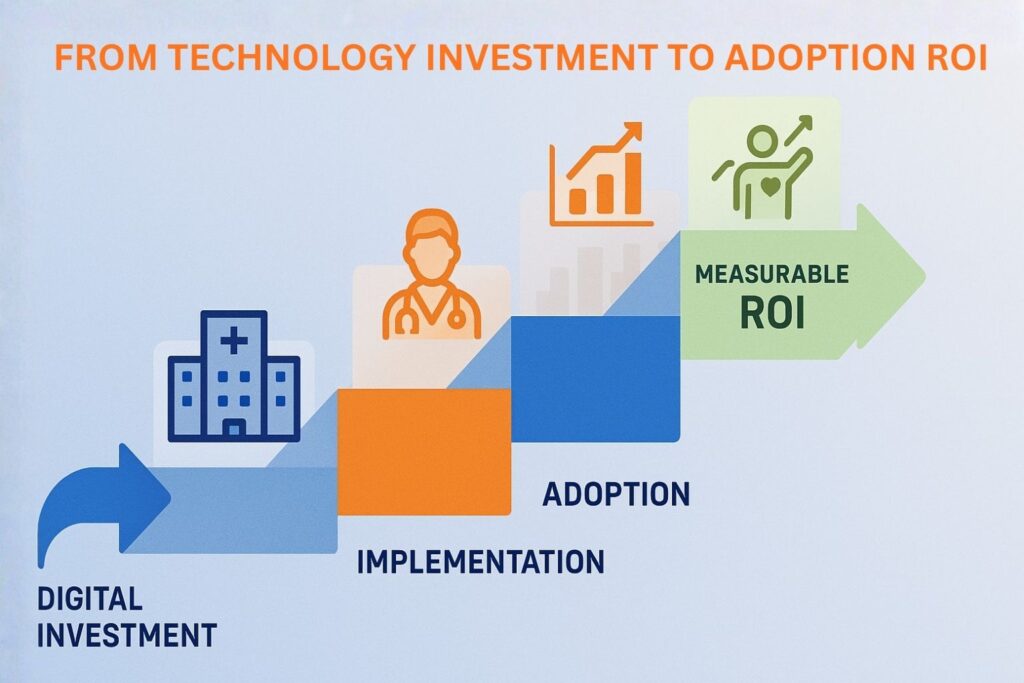
Many healthcare organizations equate digital adoption with digital transformation, but the two are not the same. Digital transformation refers to a strategic evolution in how care is delivered, governed, and measured. It encompasses technology, culture, and process change at the enterprise level. Digital implementation, on the other hand, involves the technical rollout of systems such as EHRs, patient portals, or automation tools.
Healthcare Digital Adoption occupies the middle ground between these two ideas. It focuses on how people actually use digital tools in real workflows. For example, a hospital may implement a sophisticated analytics platform, but if only a small fraction of its features are used by clinicians or administrators, the value is lost. Adoption bridges the gap between investment and impact. It turns technology from an abstract capability into a living, operational reality.
Digital adoption is fundamentally behavioral. Success depends on whether healthcare professionals can integrate new tools seamlessly into their routines. This requires intuitive design, clear workflows, and continuous contextual learning. Adoption is not achieved by sending users to a training session and expecting long-term results. Instead, it must become part of the day-to-day environment where learning and doing converge.
Organizations that achieve high adoption rates build a strong foundation for digital maturity. They develop the ability to evolve quickly as technologies and regulations change, while maintaining clinician satisfaction and patient safety.
Healthcare digital adoption affects all layers of the ecosystem. It impacts clinicians who document care, administrators who manage compliance, and executives who depend on analytics for decision-making. Effective adoption connects these layers by enabling consistent and data-driven collaboration. In contrast, fragmented adoption results in disconnected systems, redundant work, and operational inefficiency.
By recognizing adoption as a continuous capability rather than a one-time project, healthcare leaders can create organizations that adapt naturally to technology evolution rather than resist it.
Research from organizations such as HIMSS and KLAS shows that many hospitals do not fully leverage the capabilities of their major digital systems. Core tools like EHRs, analytics dashboards, and clinical decision support platforms are often implemented but not consistently integrated into everyday clinical workflows. As a result, healthcare organizations miss opportunities to improve efficiency, reduce manual work, and enhance decision-making at the point of care.
The consequence is a paradox: healthcare is one of the most technologically advanced sectors in spending, yet one of the least efficient in outcome realization. Millions are spent on digital transformation, but adoption remains shallow. When staff members revert to manual workarounds or resist using systems, transformation efforts fail to deliver measurable ROI.
The healthcare adoption gap arises from several intertwined causes:
The result is what experts call digital drag where technology exists but slows operations instead of accelerating them.
Digital drag manifests in lost productivity, clinician burnout, compliance risks, and patient dissatisfaction. When technology adds complexity rather than reducing it, it undermines trust in digital transformation. Over time, this creates cultural inertia, where staff members view new tools with skepticism.
Closing the adoption gap requires a shift in mindset. Healthcare leaders must treat digital adoption as a continuous organizational discipline, supported by infrastructure, measurement, and behavioral design, not a one-off initiative.
Healthcare operates within a uniquely complex ecosystem. Clinical workflows often involve multiple systems, such as EHRs, imaging platforms, laboratory systems, and pharmacy modules. These systems must function in real time to support life-critical decisions. Unlike other industries, healthcare cannot afford downtime for training or experimentation. This makes seamless digital integration both more difficult and more essential.
Moreover, interoperability challenges persist despite the progress encouraged by standards like HL7 FHIR (Fast Healthcare Interoperability Resources) and ONC (Office of the National Coordinator for Health Information Technology) regulations. Each system that fails to communicate effectively compounds the friction for users and increases the risk of data errors or omissions.
The regulatory environment adds another layer of complexity. Healthcare providers must comply with HIPAA (Health Insurance Portability and Accountability Act), CMS (Centers for Medicare & Medicaid Services) policies, and various state and federal mandates. Each new digital tool introduces new points of compliance and risk. Adoption programs must, therefore, balance innovation with stringent security and privacy standards.
This tension often slows adoption efforts. IT departments may focus on compliance rather than usability, creating tools that meet legal requirements but fail operationally. Successful organizations address both simultaneously through human-centered design and governance.
Healthcare professionals represent a diverse demographic, with varying degrees of comfort with digital tools. Senior clinicians may prefer legacy systems or manual workflows, while younger staff often expect intuitive, consumer-grade digital experiences. These cultural and generational gaps can lead to inconsistent adoption and process fragmentation.
To overcome this, digital transformation initiatives must include robust change management programs. Building digital literacy and confidence across the workforce requires engagement, empathy, and continuous reinforcement, not one-time communication campaigns.
The pace of technological change in healthcare is relentless. Clinicians already face documentation overload and administrative pressure. When new tools are introduced without clear purpose or user benefit, they contribute to fatigue rather than relief.
According to the American Medical Association (AMA), poor electronic health record (EHR) usability continues to be a major driver of physician burnout.
A 2025 national survey in Nature Digital Medicine found that over half of physicians reported their EHR systems do not enhance patient safety, and usability was rated at just 52% of the maximum. These results show that when digital tools add complexity instead of clarity, they directly undermine clinician well-being.
Sustainable digital adoption must therefore focus on minimizing cognitive load and aligning tools with real clinical workflows to prevent fatigue before it occurs.
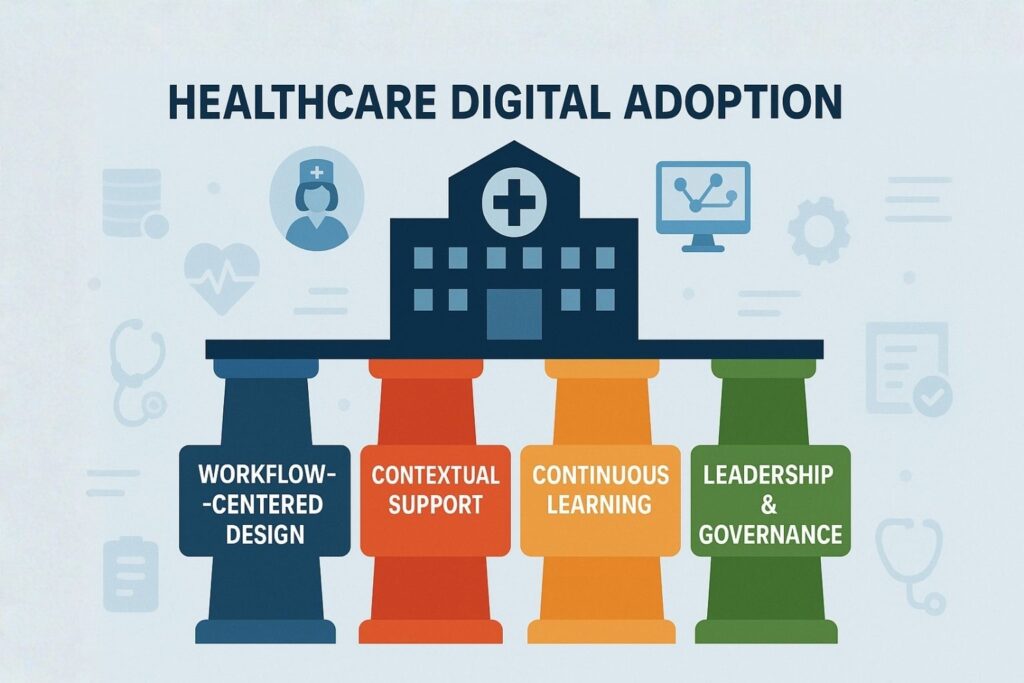
Healthcare Digital Adoption begins with understanding real-world workflows. Too often, systems are deployed based on theoretical processes that differ from actual practice. The most effective digital tools are those designed around the natural flow of care delivery.
Hospitals should invest in workflow mapping and process mining to identify friction points. This approach allows technology teams to align system interfaces with user expectations and reduce cognitive load. When digital tools integrate seamlessly into tasks like documentation, order entry, or discharge management, adoption occurs naturally.
A workflow-centered approach also improves safety. It ensures that clinicians can access the right information at the right time without excessive clicks or navigation. This focus on usability, sometimes referred to as clinical ergonomics, directly influences adoption quality.
Traditional training programs often fail because they separate learning from doing. Staff members attend training sessions and then return to their daily work weeks later, by which time most of the material has been forgotten. This problem is amplified in high-turnover or shift-based environments.
Contextual, in-the-moment learning solves this challenge. By embedding support within the digital workflow, users can receive just-in-time guidance precisely when they need it. This could include tooltips, walkthroughs, or short videos that appear as users interact with systems. These learning models dramatically improve retention and reduce errors because they are tied directly to real actions.
This principle of contextual enablement sets the stage for specialized digital adoption solutions that deliver scalable, real-time support across systems without disrupting clinical operations.
Adoption is not a static goal but a dynamic process. Over time, workflows evolve, staff members change, and new system features are introduced. Continuous learning ensures that adoption keeps pace with this evolution.
Organizations that excel in Healthcare Digital Adoption establish structured feedback loops. They collect usage data, monitor adoption metrics, and regularly update training materials to reflect user needs. This iterative process transforms adoption from an IT project into an organizational learning system.
The use of analytics-driven adoption monitoring allows leaders to identify which workflows cause the most friction and which teams require additional support. Over time, this creates a culture where improvement is continuous and data-informed.
Strong leadership is the cornerstone of sustainable adoption. Digital adoption must be owned by executives and clinical leaders, not delegated entirely to IT departments. Hospitals that appoint Chief Digital Officers (CDOs), Chief Medical Information Officers (CMIOs), or similar leadership roles are better positioned to align adoption with strategy.
Governance structures should include multidisciplinary committees that represent IT, clinical, and operational perspectives. These groups define adoption standards, track metrics, and ensure that technology investments align with organizational goals.
Most importantly, leadership must communicate the value of adoption in terms that resonate with staff. When clinicians understand how digital adoption directly supports patient outcomes and reduces their workload, engagement increases naturally.
Healthcare organizations cannot manage what they do not measure. To ensure that digital adoption creates real value, leaders must define specific success metrics that go beyond deployment counts or user logins. The true measure of Healthcare Digital Adoption lies in how well technology integrates into daily operations and enhances outcomes for patients, staff, and the organization as a whole.
Successful measurement frameworks combine quantitative metrics (system usage, time savings, error reduction) and qualitative insights (staff satisfaction, ease of use, and cultural readiness). A balanced approach allows executives to see adoption not as a binary status but as a continuum of maturity that evolves over time.
The most advanced healthcare institutions track adoption through measurable indicators aligned with clinical, operational, and financial outcomes. These include:
These metrics transform digital adoption from an abstract concept into a tangible business performance driver. When CIOs or CMIOs can correlate improved outcomes directly to higher adoption rates, technology investments gain clear executive visibility and justification.
A maturity model provides a structured way to evaluate the organization’s progress. Frameworks such as the HIMSS Digital Health Indicator (DHI) or the Gartner Digital Adoption Framework help leaders benchmark their current state and define roadmaps for advancement.
In a healthcare context, digital adoption maturity typically evolves across four stages:
Organizations that reach the integrated and optimized stages achieve what HIMSS refers to as digital health convergence where technology, people, and processes operate as a unified ecosystem.
Quantifying return on investment (ROI) in digital adoption requires linking usage data to broader organizational outcomes. For example, improved EHR adoption can reduce clinical documentation time, freeing up physician hours that can be redirected toward patient care. Similarly, better analytics tool usage can enhance population health management and improve reimbursement accuracy.
By framing adoption metrics within operational and financial language, healthcare leaders can transform digital adoption from a support function into a strategic value driver that directly contributes to mission outcomes.
Most healthcare organizations treat digital adoption as a temporary phase of a project. This short-term mindset limits potential gains. Instead, adoption must become a core enterprise capability, a built-in function of every digital initiative rather than a one-time follow-up activity.
To institutionalize adoption, leaders should embed it into strategic planning, budgeting, and governance. Every new technology initiative should include a defined adoption roadmap, complete with metrics, training models, and feedback loops. This integration ensures accountability from the start and prevents the common disconnect between IT implementation and operational uptake.
A growing number of progressive healthcare systems are establishing a Digital Adoption Office (DAO) or similar center of excellence. This unit coordinates adoption efforts across the enterprise, ensuring consistency and scalability. The DAO works collaboratively with IT, clinical operations, and education departments to standardize adoption strategies.
Key functions of a DAO may include:
This structure enables healthcare organizations to manage adoption as an ongoing process, not a sporadic effort. It also helps align adoption programs with other enterprise initiatives like cybersecurity, data governance, and interoperability.
Digital adoption does not exist in isolation. It is interdependent with other strategic priorities such as interoperability, automation, and AI readiness. When adoption is tightly integrated into these domains, healthcare organizations achieve higher operational agility and better patient outcomes.
For instance, as AI-driven tools begin to augment clinical decision-making, adoption frameworks ensure that clinicians trust and effectively use those insights. Similarly, interoperability initiatives benefit from high adoption rates because consistent data entry and standardization across systems make information exchange more reliable.
By embedding adoption into every digital priority, healthcare leaders ensure that transformation efforts are cohesive, measurable, and sustainable.
Resilience in healthcare depends on adaptability. Hospitals face unpredictable pressures from regulatory shifts to pandemics that test their ability to respond rapidly. Healthcare Digital Adoption strengthens resilience by enabling faster change implementation and reducing the dependency on external retraining efforts.
When staff can adapt quickly to new systems, workflows, or compliance requirements, the organization gains flexibility. During crises such as the COVID-19 pandemic, institutions that had invested in adoption infrastructure transitioned more smoothly to remote care and telehealth solutions. Their clinicians were already accustomed to contextual digital support, reducing downtime and error rates.
Poor adoption introduces risk. Unused or misused systems can lead to patient safety incidents, data breaches, and compliance violations. Each untrained user represents a potential weak link in operational resilience. By ensuring consistent, continuous adoption, healthcare organizations close these vulnerabilities.
Strong digital adoption also improves cybersecurity posture. When users understand systems and follow standardized processes, the risk of accidental security breaches diminishes. Adoption becomes a form of internal control that protects both clinical integrity and organizational reputation.
Resilient healthcare organizations maintain engaged and confident staff. Effective digital adoption improves the working environment by reducing frustration with complex systems and repetitive tasks, allowing clinicians to focus on patient care rather than administration.
Recent systematic research supports this connection. A 2025 systematic review in BMC Health Services Research found that EHR systems designed with workflow support, automation, and interoperability were associated with higher usability and improved medication safety. Complementary studies published in JAMIA and JAMA Network Open similarly show that more user-centered and supportive EHR environments correlate with higher physician satisfaction and reduced burnout.
By embedding usability and continuous support into digital adoption strategies, healthcare organizations can strengthen morale, enhance retention, and foster a culture of sustainable digital confidence.
To operationalize digital adoption at scale, healthcare executives can follow a structured five-stage framework that aligns technology, people, and process initiatives:
True transformation requires leadership alignment. Executives must champion digital adoption as a strategic imperative, not an operational afterthought. When CEOs, CMIOs, and nursing leaders model digital engagement, the culture follows.
Healthcare leaders should communicate the “why” of adoption linking it directly to better patient outcomes, reduced errors, and improved staff well-being. Cultural reinforcement through recognition programs and transparent reporting helps sustain motivation across departments.
Adoption-driven leadership turns technology into a unifying force rather than a divisive one. It ensures that every digital initiative strengthens the organization’s core mission of delivering high-quality, patient-centered care.
The success of modern healthcare depends not on how much technology is purchased but on how deeply that technology is adopted. Digital tools can only fulfill their potential when seamlessly integrated into the daily work of clinicians, administrators, and patients. Healthcare Digital Adoption stands at the center of this equation. It transforms digital transformation from aspiration to measurable reality.
For hospitals and healthcare providers, digital adoption is no longer optional. It is the foundation of operational excellence, patient safety, and financial resilience. Organizations that build structured, continuous adoption programs will not only achieve higher ROI on their digital investments but will also develop the agility and confidence to face future challenges.
As the healthcare landscape continues to evolve, the institutions that lead will be those that understand that the real power of technology lies not in the software itself, but in the people who use it effectively every day.
At VisualSP, we understand that true digital transformation in healthcare depends on effective adoption. Technology can only make a difference when it becomes an effortless part of how people work every day. That is why we focus on simplifying and sustaining Healthcare Digital Adoption through contextual, intelligent, and user-friendly solutions.
Our platform integrates directly into enterprise web applications, allowing clinicians, administrators, and staff to receive help at the exact moment they need it. With in-context walkthroughs, inline guidance, videos, and announcements, users stay within their workflow while learning, reducing disruptions and improving performance. This just-in-time support model helps healthcare organizations achieve faster onboarding, fewer errors, and measurable productivity gains.
What sets us apart is our AI-powered content creation capability, which automatically generates walkthroughs and guides tailored to each organization’s specific systems. This allows teams to scale adoption programs rapidly without extensive technical effort. Our AI assistant also helps healthcare teams adopt new AI tools responsibly, providing contextual guidance that ensures accuracy, privacy, and compliance. By integrating seamlessly with existing enterprise systems, VisualSP helps hospitals and healthcare providers simplify adoption, enhance communication, and accelerate transformation.
With over two million users worldwide, including trusted institutions such as NHS, VHB, and Visa, we have seen firsthand how effective digital adoption changes outcomes. We believe that healthcare professionals deserve tools that work as efficiently as they do, empowering them to focus on patients rather than processes.
If your healthcare organization is ready to close the adoption gap and turn technology into a competitive advantage, we invite you to explore how VisualSP can help.
Fuel Employee Success
Stop Pissing Off Your Software Users! There's a Better Way...
VisualSP makes in-app guidance simple.